John Doe
General SurgeonPretium saepe pariatur ornare cillum repudiandae inceptos iaculis cumque vulputate sequi neque quos exercitation aliquip interdum, veniam? Aute error, elit!
Pretium saepe pariatur ornare cillum repudiandae inceptos iaculis cumque vulputate sequi neque quos exercitation aliquip interdum, veniam? Aute error, elit!
Other gastrointestinal surgery involves procedures on any part of the digestive tract, from the esophagus to the rectum, to treat various conditions affecting the GI system. It is found that due to change in lifestyle there is an increase in gastrointestinal diseases. Here’s an overview to understand gastrointestinal surgeries in detail.
Read on!
GI surgery may be recommended for conditions including:
Tumors in the stomach, intestines, colon, or other Gastrointestinal part. Cancer cases are increasing, boosting the rate of gastrointestinal surgeries.
Inflammation of gallbladder due to oxalate crystal can be painful, that needs immediate medication and surgical treatment. These Gallstones or inflammation often require gallbladder removal.
In this condition the abdominal area bulges out near the abdomen. Repairing abdominal or inguinal hernias, where an organ pushes through a weak spot in the muscle wall.
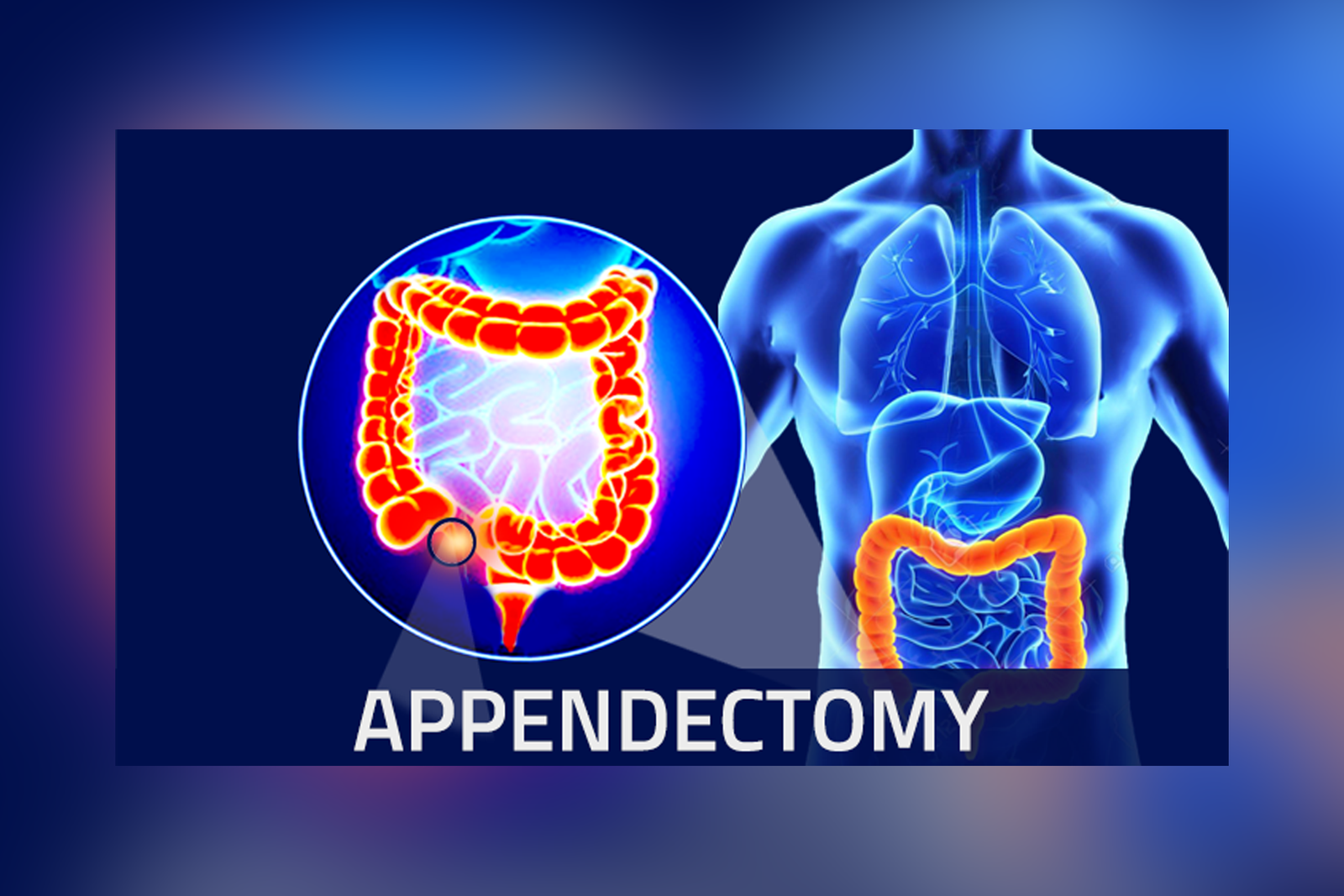
Appendix is a vestigial organ in the body. This organ can hurt any individual if inflamed. Then Removal of the appendix is recommended if it becomes inflamed and painful.
Due to old age, arteries exert pressure on the walls that causes clotting of blood and formation of clot disrupt the flow, Removal or bypass of blockages in the intestines.
Surgical treatment of complications from severe cases.
This condition can cause in old age patients due to lack of motility, acid reflux is so discomforting if chronic. For chronic acid reflux (gastroesophageal reflux disease) that doesn’t respond to medication, surgery can repair or reinforce the esophagus.
If large blockages are found then it involves large incisions to access the organs, usually for complex or large tumors, extensive resections, or emergency cases which need to be operated on emergency basis.
Laparoscopic surgery effortlessly inserts a laparoscope in the body for clear visualization of the internal condition. Small incisions allow a camera and instruments to be inserted, reducing recovery time and scarring. Commonly practice for gallbladder removal, appendectomy, and hernia repair.
Uses an endoscope (a flexible tube with a camera) for diagnostic and therapeutic procedures. It is often used for early-stage cancers, polyps, that helps in designing treatment regimens for the patient in the early stage itself and other minor conditions without incisions.
Uses robotic-assisted surgery systems for treatment and procedures. Its results are precise and controlled, especially in complex surgeries requiring delicate movements, like rectal or esophageal procedures.
Gastrointestinal surgeries reduce recovery time, less pain, smaller scars, and often faster return to normal activities with least efforts, especially with minimally invasive techniques that are easily done by the specialist doctors.
As with any surgery, risks include infection, bleeding, and reactions to anesthesia, along with the specific risks tied to the area being operated on, such as bowel leakage or strictures.
Post-surgery, it very important to take proper care of wounds and the operated areas, recovery include,
Make sure to eat light, that is easy to digest .A soft or liquid diet may be needed initially to ease digestion. After some period of time one can switch to leafy vegetables and carbohydrates.
Make sure you avoid heavy lifting and strenuous activity for a certain period of time after the surgery. It can harm the operated wounds, which will eventually prolong the recovery process.
Doctors prescribe medicines after the surgery that helps to heal wounds fast and also helps in pain management, antibiotics to prevent infection, and medications to support digestion.
Gastrointestinal surgeries are specialized and often require careful coordination with other providers, like gastroenterologists, for pre- and post-operative care. It’s completely the doctor’s decision to decide whether to perform open surgery or minimally invasive procedure depending on the health condition offered by the patient.
In most of the cases gastrointestinal surgeries are carried out using minimally invasive techniques, these are simple and accurate that helps to detect and treat diagnosed diseases rapidly.
GI surgeries are generally safe, especially with advances in minimally invasive techniques. However, all surgeries carry some risk, including infection, bleeding, blood clots, and potential issues specific to the area treated (e.g., leakage or strictures in the bowel).
In some cases, non-surgical options like medications, lifestyle changes, and dietary adjustments can manage conditions like acid reflux, mild hernias, and minor obstructions. However, severe or life-threatening conditions often require surgical intervention.
Some surgeries, especially those involving removal of part of the stomach, intestines, or gallbladder, can impact digestion. Dietary adjustments or supplements may be necessary, and some patients experience changes in bowel habits.
Follow your doctor’s advice closely, attend follow-up appointments, adhere to dietary guidelines, avoid smoking and alcohol, and monitor for any post-surgical symptoms like fever, severe pain, or unusual discharge.
GI surgeries are generally safe, especially with advances in minimally invasive techniques. However, all surgeries carry some risk, including infection, bleeding, blood clots, and potential issues specific to the area treated (e.g., leakage or strictures in the bowel).
In some cases, non-surgical options like medications, lifestyle changes, and dietary adjustments can manage conditions like acid reflux, mild hernias, and minor obstructions. However, severe or life-threatening conditions often require surgical intervention.
Some surgeries, especially those involving removal of part of the stomach, intestines, or gallbladder, can impact digestion. Dietary adjustments or supplements may be necessary, and some patients experience changes in bowel habits.
Follow your doctor’s advice closely, attend follow-up appointments, adhere to dietary guidelines, avoid smoking and alcohol, and monitor for any post-surgical symptoms like fever, severe pain, or unusual discharge.
